Vitreo Retinal Services
COMMON DIAGNOSTIC TESTS:
- Fundus Photography
Color photographs of the back of the eye - Fluorescein Angiography (FFA) -Spectralis HRA system
a diagnostic procedure that photographs the blood circulation of the retina. This involves injection of a dye called fluorescein into a vein in the arm or hand. - Spectral Domain Optical Coherence Tomography (SD-OCT) – Spectralis
This is a diagnostic procedure similar to the CT scan of the brain. It uses a beam of light and its reflection to obtain cross-sectional images that provide information about the different layers of the retina. - Ultrasonography (B-Scan)
This procedure involves use of high-frequency sound waves to examine the eye when the normal view is obscured by hemorrhage or cataracts. - Visual Field Analysis
Measurement of the full extent of the area visible to an eye that is fixating straight ahead.
LASERS PASCAL (Pattern Scan Laser)
Trinity Eye Hospital boasts of an advanced version of laser photocoagulation system. The PASCAL (Pattern Scan Laser) Photocoagulator is a new system designed to treat retinal diseases. There are several benefits with the Pascal laser compared to the conventional laser. Most of the laser can be done in one or two sittings. This in turn reduces the number of patient-visits to the hospital. The procedure also significantly reduces the discomfort associated with conventional laser, and therefore patient tolerance is much better. Pascal laser can be used in most situations where conventional laser is indicated.
Indirect Ophthalmoscopic Laser Delivery System (LIO)
This laser delivery system is mainly used for peripheral retinal lesions, e.g. horse shoe tear (HST), lattice degeneration, retinal holes, Retinopathy of prematurity (ROP) or pan retinal photocoagulation for vascular retinopathy in a hazymedia. CRYOTHERAPY
Cryotherapy is a second way of treating retinal tears apart from laser. An extremely cold probe is used to “freeze-burn” a small area on the outside of the eyeball that overlies the retinal tears. The purpose is to seal the tears and create an eventual scar that will “stick” the retina to that spot.PNEUMORETINOPEXY
Pneumoretinopexy is a method of treating selected cases of retinal detachments. A gas bubble is injected into the eye after applying cryo spots to the area of retinal tear. The patient is expected to maintain a certain posture after the procedure for about a week to ten days. Also, he is not allowed to travel by air during this period.ANTERIOR CHAMBER / VITREOUS TAP
A very small amount of fluid from inside the eye is removed in cases of suspected infection or persistent inflammation in the eye. This fluid is then analyzed microbiologically and biochemically to aid in the diagnosis.DIABETIC RETINOPATHY
Diabetes mellitus is emerging as a major public health problem in India. It is a multisystem disorder which affects the heart, kidneys, peripheral nerves and the eyes. Involvement of the retina is called diabetic retinopathy, and can lead to blindness. In patients with more than twenty years of diabetes, nearly all patients with type I diabetes (insulin-dependent) and more than 60% of those with type II diabetes (non-insulin dependent) will have some degree of retinopathy. This also depends on how well the disease has been controlled. Trinity eye Hospital offers comprehensive facilities for the medical and surgical management of diabetic retinopathy.What is diabetic retinopathy?
Diabetic retinopathy is an eye problem that can be caused by either type 1 or type 2 diabetes mellitus. Retinopathy occurs when diabetes damages the tiny blood vessels in the retina. The weakened blood vessels may leak fluid and blood.Who are at risk for developing diabetic retinopathy?
Those with poorly controlled blood sugar levels are at a high risk of developing diabetic retinopathy. In addition, high blood pressure, high cholesterol, anemia, kidney disease and pregnancy can all place a patient at greater risk of suffering from diabetic eye disease.How frequently should I get my eye examined?
If you have diabetes, you should get a yearly examination by your ophthalmologist. Once you develop diabetic retinopathy, your ophthalmologist may advise further investigations or treatment. A periodic follow up as advised by your ophthalmologist is mandatory. The frequency of these follow up visits is decided based on the severity of the disease.What are the symptoms of diabetic retinopathy?
There may be no symptoms in the early stages, especially when the central portion of the retina is not involved. As the retinopathy progresses, you may have:
- Blurred vision
- Floaters, which can look like black spots, little threads, or cobwebs
- Bleeding in the eye causing sudden loss of vision
- Temporary or permanent loss of vision.
- Pain is not a common feature of the disease.
What are the types of diabetic retinopathy?
There are two forms of diabetic retinopathy: non-proliferative (NPDR) and proliferative (PDR). Non-proliferative diabetic retinopathy refers to the early stages of the disease, while proliferative diabetic retinopathy refers to the severe, progressive stage.Macular edema:
The fluid and exudates collect in the macula, the central part of the retina that helps us in fine central vision.What is laser treatment? Will I regain my vision after laser treatment?
The aim of this treatment is to protect central vision. It does not restore lost vision, but it can prevent further deterioration, which is why early diabetic retinopathy diagnosis through periodic eye examination is imperative. Laser photocoagulation involves tiny burns to seal the capillaries. This may cause small spots to appear in your field of vision after the procedure. These spots generally fade and disappear with time. Some patients may experience difficulties in dim illumination and while reading following multiple sittings of laser treatment.How many sittings of laser treatment are required?
With the PASCAL® (Pattern Scan Laser), the entire session can be completed in one or two sittings. It may however vary from patient to patient. The severity of diabetic retinopathy plays an important role in deciding the number of sittings required.What are Anti VEGF agents, and what is their role in managing diabetic retinopathy?
Anti VEGF agents (Avastin, Razumab, Accentrix, Lucentis, Eylea) are emerging as the new modality of treatment for various stages of diabetic retinopathy. These agents are injected into the eye (intravitreal injection). They are commonly used in diabetic maculopathy and proliferative diabetic retinopathy. They may also be used as an adjunct before surgery for diabetic vitreous hemorrhage and retinal detachments.What is vitrectomy?
Vitrectomy is a surgical procedure in which cloudy, blood filled vitreous and scar tissue causing tractional retinal detachments are removed from the eye.INTRAVITREAL INJECTIONS
This is an injection into the vitreous, which is the jelly-like substance inside your eye. It is performed to place medicines inside the eye near the retina. Intravitreal injections are used to deliver drugs to the retina and other structures in the back of the eye, thus avoiding effects on the rest of the body. Common conditions treated with intravitreal injections include diabetic retinopathy, macular degeneration, retinal vascular diseases and ocular inflammation.PROCEDURE
The actual procedure may take around 10 minutes and is carried out in minor operation theatre. You will be made to lie down in a comfortable position and anaesthetic (numbing) drops will be applied in your eye. Your eye will be cleaned with an iodine antiseptic solution. A speculum is inserted and the medicine injected into the vitreous. You may experience a mild discomfort during the procedure. Antibiotic eye drops need to be instilled for a week.The doctor will see you within 3 days for inflammation or increase in intraocular pressure.
Instructions following an intravitreal injection
- There are no special precautions except to avoid rubbing the eye.
- Instill the antibiotic eyedrops 4 times a day for 1 week.
- You can also take mild painkillers to alleviate any discomfort during the first few days.
Normal effects following an intravitreal injection
- A subconjunctival haemorrhage (bloodshot eye) usually occurs at the injection site. This will gradually fade within 7 to 10 days.
- Your vision may become slightly more blurred immediately after the injection. There may also be some floaters in your vision.
- You may experience mild discomfort for a few days after the injection. This discomfort should be relieved by mild painkillers.
Warning symptoms following an intravitreal injection
Although rhegmatogenous retinal detachment and cataract are potential complications of intravitreal injection, the most feared complication is endophthalmitis i.e. infection inside the eye (rates typically less than 1%). The warning symptoms of this complication are rapid onset of:
- Increasing eye pain.
- Increasing redness of the eye.
- Greatly decreased vision.
In AMD, diabetic retinopathy and retinal venous occlusion, there are increased levels of vascular endothelial growth factor (VEGF) in the eye which gives rise to new vessels and macular edema. To counteract this, an anti VEGF injection is given. The anti VEGF injections are available as Lucentis, Macugen and Avastin (off label use). Anti VEGFs can rarely cause cerebrovascular events in the form of stroke or myocardial infarction (heart attack). Hence in patients who have a risk or history of ischemic heart disease or stroke, Macugen is preferred as it has less chance of causing such events.
These injections might have to be repeated more than once, depending upon the response of the eye.
Intravitreal triamcinolone acetonide
Triamcinolone acetonide is a long acting steroid which is given in the eye in cases of macular edema secondary to diabetes, retinal venous occlusion or uveitis (ocular inflammation). You may feel black spots floating in front of eye, which is due to drug deposit in the vitreous. This will reduce over a period of few weeks as the drug is absorbed.Triamcinolone may cause an increase in eye pressure (glaucoma) or cataract (clouding of the lens). The intra ocular pressure can increase in 30% people who undergo the injection. The pressure in your eyes will be checked at every visit and eye drops prescribed if the pressure increases significantly. This increase is transient, and these drops can be discontinued after some time. Cataracts are not a serious problem for the first few months after the injection, but over 50% of treated eyes will eventually develop significant cataract if triamcinolone has to be repeated.
OZURDEX INTRAVITREAL IMPLANT
This is an intravitreal steroid implant which is approved for the treatment of macular edema secondary to retinal venous occlusion. It has recently been approved by the US FDA for use in eyes with macular edema secondary to uveitis (ocular inflammation). This implant remains in the vitreous cavity for a longer duration compared to the intravitreal injections, and hence unlike other intravitreal injections, the effect of Ozurdex lasts minimum 3 months following a single injection.VITREORETINAL SURGERY
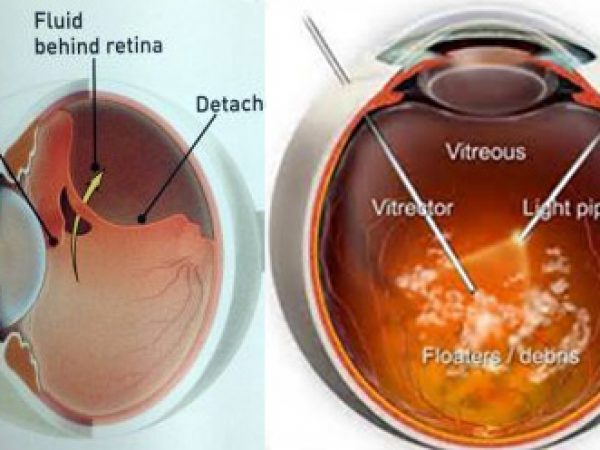
RETINAL DETACHMENT
RETINAL DETACHMENT
What does retinal detachment mean?
The retina is the light-sensitive layer of tissue that lines the inside of the eye and sends visual messages through the optic nerve to the brain. When the retina detaches, it is lifted or pulled from its normal position. If not promptly treated, retinal detachment can cause permanent vision loss.Who is at risk for retinal detachment?
A retinal detachment can occur at any age, but it is more common in people over 40 years. It affects men more than women.A retinal detachment is also more likely to occur in people who:
- Are extremely nearsighted (high myopes)
- Have had a retinal detachment in the other eye
- Have a family history of retinal detachment
- Following cataract surgery, there is a 1% to 2% chance of developing a retinal detachment.
- Have other eye diseases or disorders, such as retinoschisis, uveitis, degenerative myopia, or lattice degeneration
- Have had an eye injury
What are the alarming symptoms of retinal tear and detachment?
- Floaters which are little “cobwebs” or specks that float about in your field of vision
- Light flashes in the eye
- Sudden blurry vision
- An area of dark vision, like a curtain or a veil coming from above or below or from the sides.
What are retinal holes / tears?
Holes are small circular defects in the retina. Tears are due to a flap of retina being pulled off as the vitreous shrinks.What do you mean by laser and cryo therapy?
Laser therapy (Diathermy):Laser is a beam of light that is converted to heat when it hits the retina. This welds the retina to the underlying choroid.
Cryo treatment:
Cryotherapy refers to a cold probe that freezes the tissue around the tear causing the retina and choroid to stick together.
WHAT IS VITRECTOMY?
The vitreous is removed, therefore the name “Vitrectomy”. The lack of vitreous does not affect the functioning of the eye. Trinity Eye Hospital has the latest and the most sophisticated surgical equipments. Micro incision and sutureless (23/25 gauge) vitrectomy (MIVS). The advantage of this surgery is the absence of stitches in the eye; hence the post-operative recovery is faster.The surgeries performed in our department are as follows :
- Scleral Buckling
- Vitrectomy for retinal detachments, epiretinal membrane, macular hole, vitreomacular traction, vitreous hemorrhage, parasitic cysts, dislocated nucleus, dislocated intra ocular lens
- Vitrectomy for diabetic retinal detachment
- Scleral fixated IOLs
- Surgery for trauma-related conditions
- Subretinal surgery
- Surgery for intra ocular infections
- Pneumoretinopexy
AGE RELATED MACULAR DEGENERATION (AMD)
The retina is the light-sensitive tissue lining the back of the eye. The macula is the part of the retina that is responsible for your central vision, allowing you to see fine details clearly. Many older people develop macular degeneration as part of the body’s natural aging process. This is called age-related macular degeneration (AMD).What are the symptoms of AMD?
With macular degeneration, you may have symptoms such as blurred vision, dark areas or distortion in your central vision, and sometimes, permanent loss of your central vision. The peripheral vision is usually spared. Early symptoms are loss of clarity while reading and distortion of objects. With advanced macular degeneration you may fail to recognize a person’s face. AMD usually affects both eyes, although not necessarily to the same extent. What are the types of AMD?
AMD is of two types :Dry AMD
With dry macular degeneration, vision loss is usually gradual. These patients need to monitor their central vision regularly. If you notice any change in your vision, you should tell your eye doctor right away, as the dry form can change into the more damaging form which is wet (exudative) macular degeneration. While there is no medication or treatment for dry macular degeneration, some people may benefit from vitamin supplements (anti-oxidants).
Wet AMD
About ten percent of people who have macular degeneration have the wet form. This can cause more damage to your central vision than the dry form. Wet macular degeneration occurs when abnormal blood vessels begin to grow underneath the retina. This blood vessel growth is called choroidal neovascularization (CNV) because these vessels grow from the layer under the retina called the choroid. These new blood vessels may leak fluid or blood, blurring or distorting central vision. Vision loss from this form of macular degeneration may be faster and more noticeable than dry AMD.
Can AMD be prevented?
The exact cause of AMD is unknown. A healthy life style without smoking and a good diet may reduce the risk.
Can AMD be treated?
There is no treatment for dry AMD, although high dose multivitamin combination has been shown to decrease the risk of visual loss. There are a few treatment options for wet AMD although the best outcomes occur when this disease is detected early. These include thermal laser, photodynamic therapy, anti-VEGFs or combinations of these. Not all patients may benefit from these, and treatment may not prevent further vision loss.How will I know I have AMD?
Early reporting of new distortion or blurred vision should be reported to the eye doctor. The earlier the disease is detected, the more amenable it is to treatment. The earliest symptom is distortion of straight lines, making a grid pattern appear distorted.Other facilities:
- Photodynamic therapy(PDT)
- High speed vitrectomy machine